Test How Your Invisible Gut Bacteria Affects Your Health
The reason you should test how your gut bacteria affects your health is pretty straightforward — those bugs impact nearly every aspect of your well-being, so learn how to find out if yours are working for or against you.
Updated 7/18/2022
This post is about how gut bacteria affects your health, but some context would be helpful before I delve into that.
Did you know that your amazing human body has 12 basic biological systems that must function reasonably well for us to experience health and vitality?
These 12 are: the cardiovascular system, the digestive system, the endocrine system, the immune system, the integumentary system, the lymphatic system, the muscular system, the nervous system, the reproductive system, the respiratory system, the skeletal system, and the urinary system.
All of these systems work in concert to make sure that our bodies work correctly:
- The cardiovascular/circulatory system transports blood, oxygen, and nutrients throughout the body. The digestive system takes in and processes food.
- The endocrine system produces hormones that regulate metabolism, growth and development, tissue function, sexual reproduction, sleep, and mood.
- The immune system fights infection.
- The integumentary system protects the body from outside damage.
- The lymphatic system connects the lymph nodes in our bodies and helps the circulatory and immune systems. The muscular system allows us to move.
- The nervous system transmits signals through the body and controls voluntary and involuntary actions. The reproductive system allows us to have sex and children.
- The respiratory system enables us to take in oxygen and expel carbon dioxide as we breathe.
- The skeletal system gives our bodies a framework and supports the systems.
- The urinary system expels waste.
But there’s one “system” that’s vitally important to our well-being, yet not included in those 12. In fact, you probably didn’t miss it, or think about it. Odd that you could not live without it and yet it’s not really you, but a part of you.
I’m referring to our microbiota.
We have an intricate, essential symbiotic relationship with single-cell bacteria — perhaps 100 trillion of them — that live in every nook and cranny on and in us, particularly within our gastrointestinal track.
Together, these microbiota create an environment called the microbiome, and yours must be healthy in order for you to be healthy.
So, how can you know how all your buggies are affecting your health?
How can you know if your issues with weight gain, brain fog, digestion, allergies, ulcers, bowel disease, immune function — even Parkinson’s disease — may be a result of a lack of beneficial bacteria and too much harmful bacteria?
Your microbiota can either cause or amplify nearly all chronic diseases. It’s time to find out if yours is friend or foe. You can do that with tests offered by Viome.
In this article, you’ll discover:
- What is “Dybosis” and how it and gut bacteria affects your health;
- Why the little-known Firmicutes to Bacteroides Ratio so important;
- How the Firmicutes to Bacteroides Ratio influence body composition (body fat);
- Which are the best foods and supplements to build a healthy microbiome; and
- How and why you should use the discounts here offered to get yourself tested.
Let’s dig in…
The Essential Bacterial Balancing Act
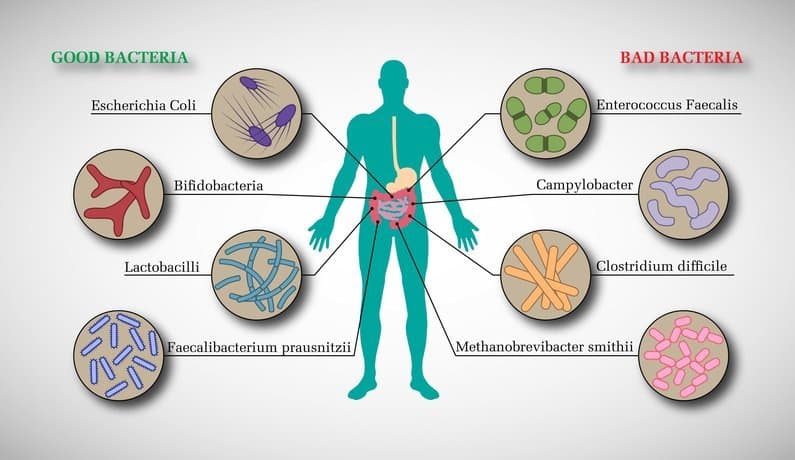
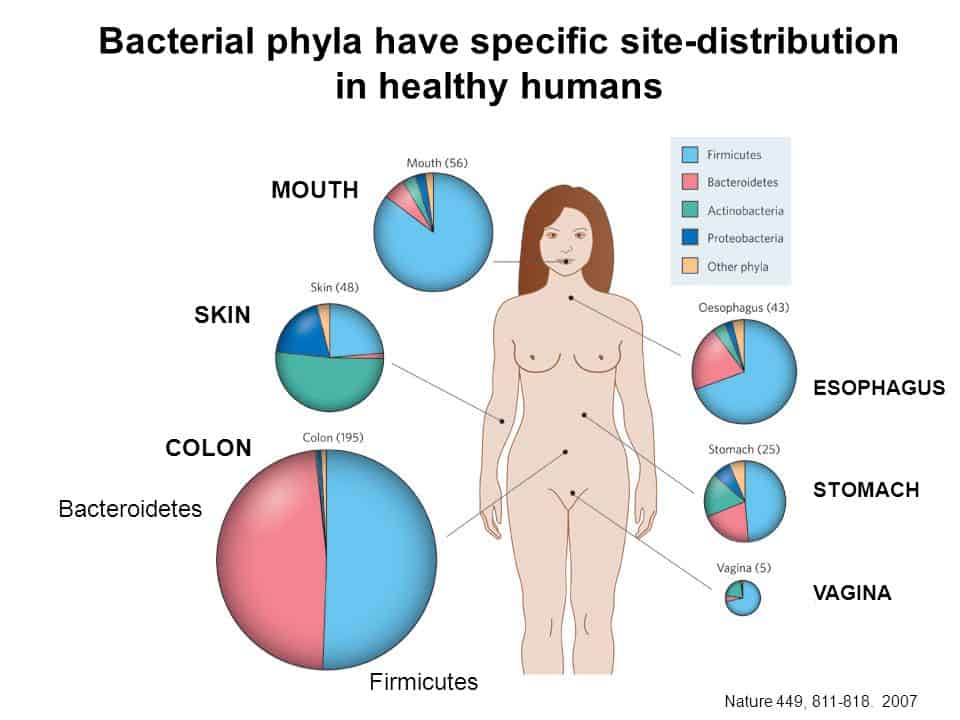
Salveo Diagnostics has a good review of why your microbiome is important and how you can ensure it’s healthy, which I’ll summarize. The focus here is on the bacteria that resides in our gastrointestinal tract, primarily our gut, and the effects that an unbalanced ratio of the two main types (“phyla“) of bacteria can bring on can damage the gut lining and lead to chronic diseases, among other unsavory things.
In this section, we’ll first look at why a healthy gut microbiota is vital to our well-being, and then examine an important relationship — the Firmicutes to Bacteroidetes ratio.
How Dysbiosis Impacts Your Health
A healthy gut microbiota pitches in and helps our body do many essential things; for instance they can:
- Establish and keep up our immune system,
- Fend off opportunistic pathogens,
- Extract nutrients and energy from foods we cannot digest (e.g., dietary fiber),
- Produce vitamins, and
- Stimulate communication between the gut and brain. 1-5
Ingesting enough fiber is a relatively quick and easy way get on the right microbial track, as it’s exceedingly important to gut health.
The beneficial end-products of fiber fermentation are short-chain fatty acids (SCFAs). These fatty acids nourish the gut lining and regulate food intake, and improve inflammatory tone, resilience to stress and insulin signaling.1,2,6,7
Dietary fiber helps create microbiota diversity, because such diversity depends on both a diet rich in fiber and the quick colonic transit time it enables.2,7
Dysbiosis is an undesirable shift in the microbiota composition, resulting in an imbalance between protective and potentially harmful microbes that can damage the gut lining and lead to chronic diseases.2,9
In addition to pathogens and toxins, a high-fat, high-sugar, low-fiber (standard Western) diet may induce dysbiosis and cut microbial diversity.2,10
Over time, dysbiosis can cause impaired glucose and lipid metabolism, aberrant immune responses, intestinal permeability, and metabolic endotoxemia (toxins impairing metabolic function),3,9 paving the way for cardiometabolic, autoimmune, and other inflammatory disorders.1-3
Further, gastrointestinal imbalance is compounded by other, all-too-common factors, such as a sedentary lifestyle, high stress levels, excessive alcohol intake, and gut-damaging medications.4,11-13
Chronic dysbiosis can alter gut pH and disrupt the epithelial mucus layer, creating space for pathogens to flourish.2,14
To put it in a nutshell, untreated intestinal dysbiosis may underpin a variety of chronic diseases1,2,9:
- Inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and colon cancer
- Gastric ulcers, nonalcoholic fatty liver disease, and cardiometabolic diseases
- Allergic disorders and autoimmune disorders (e.g., celiac disease, rheumatoid arthritis, eczema)
- Mood disorders (e.g., anxiety, depression)
The impression I’m trying to make is that your gut bacteria affects your health in a myriad of ways, and that many of us have lifestyle habits (like poor diets and couch potato tendencies) that favors the propagation of harmful types of bacteria.
The Important Firmicutes to Bacteroides Ratio
In humans, about 90% of gut bacteria are represented by two phyla—Firmicutes (60–80%) and Bacteroidetes (15–30%).15,16
The Firmicutes phylum encompasses more than 250 genera, including Lactobacillus and Clostridium, while Bacteroidetes includes around 20 genera, the most abundant being Bacteroides.
Both phyla produce beneficial SCFA from indigestible carbohydrates that reach the colon, with Firmicutes being the main butyrate-producers and Bacteroidetes producing mainly acetate and propionate.16
What you need to know about Butyrate-producing bacteria is that they’re important for a healthy colon and when altered contribute to emerging diseases, such as ulcerative colitis and type II diabetes. A study published in 2015 found that butyrate increases mitochondrial activity, prevents metabolic endotoxemia, improves insulin sensitivity, possess anti-inflammatory potential, increases intestinal barrier function and protects against diet-induced obesity.
(I think we all want more of that stuff.)
What you need to know about Propionate-producing bacteria, says that same study, is that it inhibits cholesterol synthesis, thereby antagonizing the cholesterol increasing action of acetate, and to inhibit the expression of resistin in adipocytes.
What you need to know about Acetate-producing bacteria is that it can contribute to obesity, among other unwanted outcomes.
Thus, we have the largely beneficial Bacteroidetes and the Firmicutes which can be both beneficial and harmful. The key is the ratio of one to the other.
A shift in the Firmicutes to Bacteroidetes ratio (F/B ratio) may be influenced by various factors and conditions:
- Various factors such as changes in nutrition, digestive secretions, use of prescription medications, and alterations in gut transit time all influence a decrease in the F/B ratio and microbial diversity with age.16,17
- Higher F/B Ratios have been associated with a standard Western diet.17 Evidence suggests that Bacteroidetes communities can shift according to dietary modulation and weight change, whereas Firmicutes numbers are more dependent on one’s genetic makeup.15,17
- Antibiotic-associated diarrhea, Crohn’s disease, and ulcerative colitis have been correlated with decreases in Firmicutes strains, a concomitant increase in Bacteroidetes (low F/B ratio), and a reduced gut biodiversity.9,18Although obesity and energy intake can affect the microbiota, studies fail to show a consistent relationship with the F/B ratio.19However, metabolic comorbidities have been associated with a higher ratio in obese patients.20
- Dysbiosis has been suggested to play a role in the development of type 2 diabetes (T2D).1-3 Patients with T2D have a lower F/B ratio than nondiabetic controls with worsening glucose tolerance as the F/B ratio decreases.21
Read my article, The 4 Food Solution to the 100 Trillion Reasons You’re Fat, Sick and Depressed.
The uptake on this is that it’s not the case where the ideal is a high or low F/B ratio, but a moderate, balanced one.
Salveo Diagnostics offers this interpretation of the F/B ratio:
| Low | Mildly Low | Optimal | Mildly High | High |
| ≤ 0.2 | 0.3 | 0.4 – 3.7 | 3.8 – 20.9 | ≥ 21.0 |
The range to strive for is just below 50/50 in favor of Bacteroidetes.
The pertinent question, then, is:
How do you get your main bacterial phyla — Firmicutes and Bacteroidetes — to play together nicely at the ratio of 0.4 to 3.7?
The answer to that is next up.
How the Firmicutes to Bacteroides Ratio Influence Body Composition
Along with the other mammals, we humans have two main types of friendly gut bacteria: Bacteroidetes and Firmicutes. If you’re overweight or obese, however, one is decidedly unfriendly.
The evidence that the gut flora in lean patients is different from that in obese people. It appears that the more body fat you have, the higher the numbers of Firmicutes are relative to Bacteroidetes.
Simply put:
Obese people seem to have more Firmicutes than Bacteriodetes in their guts.
If you put people on a diet for a year, you can actually change the Firmicutes-to-Bacteroidetes proportion. Give people antibiotics and obesity could be triggered because antibiotics changes the mix of beneficial to harmful microbes in your microbiome.
How can you improve the Firmicutes-to-Bacteroidetes ratio?
There’s a class of phytonutrients, called polyphenols, that do two things: they preferentially feed Bacteriodetes, while at the same time suppressing the growth of Firmicutes.
Researchers experimenting with certain foods packed with polyphenols, like apple cider vinegar, green tea and blueberries have seen beneficial changes in gut flora, which can alter the balance between the two groups of Bacteroidetes and the Firmicutes bacteria, in the favor of Bacteroidetes.
Watch Dr. Micheal Gregor explain this:
Feed Your Bugs Right
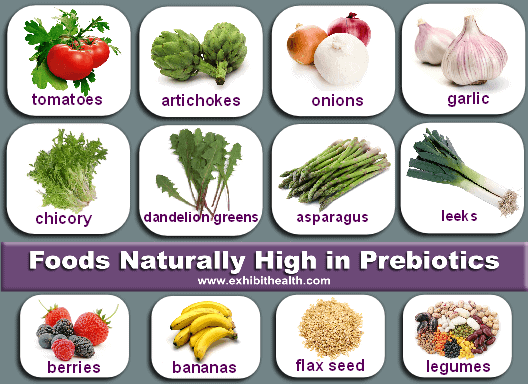
For ideal balance of the gut microbiota, consider a diet that is low in refined carbohydrates and processed foods, rich in fiber, essential fatty acids, and phytonutrients, with a variety of fresh fruits and vegetables, beans (legumes), nuts, and whole grains. Depending upon clinical context, the following suggestions may also help restore the microbiota:
- Specific pharmaceutical or botanical medications may be taken under the guidance of a qualified clinician for the treatment of bacterial, fungal, or parasitic infections.
- Abstinence from gut-damaging medications (e.g., antibiotics, nonsteroidal anti-inflammatory drugs, proton-pump inhibitors, oral contraceptives) and alcohol.12,13
- Probiotics, especially Lactobacilli and Bifidobacteria, help restore GI balance; they activate anti-inflammatory pathways, regulate gut contractility and calm IBS symptoms, improve weight control and insulin sensitivity, and reinforce intestinal barrier integrity.24,25 “Reseeding” the dysbiotic gut with these friendly bacteria may prevent pathogens taking up residence. Probiotics can be found in fermented foods (e.g., yogurt, miso, tempeh, and sauerkraut) or taken as supplements.
- Prebiotics, food ingredients that feed the gut flora, can augment the benefits of probiotics and include bran, resistant starch, and oligosaccharide-containing foods such as onions, garlic, leeks, chicory, asparagus, tofu, and bananas.23 Supplemental prebiotics may help patients with low levels of beneficial short chain fatty acids.
- Low stomach acid (often resulting from treatment with gastric acid suppressants) and pancreatic insufficiency may exacerbate the effects of dysbiosis by impairing digestion and assimilation of food.4 If fecal elastase (a diagnostic test for pancreatic function) levels are low, consider supplemental pancreatic enzymes. Drinking warm water containing fresh lemon juice before meals may aid digestion by stimulating gastric acid secretion.
- Patients with dysbiosis may benefit from vitamin and mineral supplements that address associated nutrient deficiencies. The MegaFood brand is exceptional.
- Regular physical exercise lowers inflammation, and can increase microbial diversity and decrease transit time.11
Click here to see footnoted references.
- Marchesi JR, et al. Gut 2016;65:330–339.
- Chan YK, et al. Ann Nutr Metab 2013;63(Suppl 2):28–40
- Nicholson JK, et al. Science 2012;336:1262–1267
- Cresci GA, et al. Nutr Clin Pract 2015;30:734–746.
- Di Mauro A, et al. Ital J Pediatr 2013;39:15.
- Corfe BM, et al. Proc Nutr Soc 2015;74:235–244.
- Lozupone CA, et al. Nature 2012;489:220–230.
- David LA, et al. Nature 2014;505(7484):559–563.
- Carding S, et al. Microb Ecol Health Dis 2015;26:26191.
- Hold GL. BMJ 2014;16(1):5–6.
- Cerdá B, et al. Front Physiol 2016;7:Article 51.
- Khalili H, et al. Gut 2013;62:1153–1159.
- Engen PA, et al. Alcohol Res 2015;37(2):223–236.
- Duncan SH, et al. Environ Microbiol 2009;11(8):2112–2122.
- Goodrich JK, et al. Cell 2014;159:789–799.
- Mariat D, et al. BMC Microbiol 2009;9:123.
- Voreades N, et al. Front Microbiol 2014;5:1–9.
- Ott SJ, et al. Gut 2004;53:685–693.
- Tagliabue A, Elli M. Nutr Metab Cardiovasc Dis 2013;23:160–168.
- Louis S, et al. PLoS One 2016;11(2):e0149564.
- Larson N et al. PLoS One 2010;5(2):e9085.
- Martinez I, et al. ISME J 2013;7:269–280.
- Conlon MA, Bird AR. Nutrients 2015;7:17–44.
- Ebner S et al. World J Gastroenterol 2014;20(43):16095–16100.
- Le Barz M, et al. Diabetes Metab J 2015;39:291–303.
How To Check Your Microbiome to Learn How Your Gut Bacteria Affects Your Health
The viome microbiome test reveals the precise food and supplements you need to restore your microbiome health.
You can either spend eight-plus years getting a doctorate in microbiota, poo on a petri dish, scrape off a sample and spend your days seeking and categorizing the bacteria found there — and still have no idea if your findings are correct, because these days accuracy comes from DNA sequencing — or you can open your wallet and buy one of three tests offered by Viome.
Three tests are offered by Viome:
Full Body Intelligence™ — Food + supplement recommendations determined by over 50 health scores and based on an analysis of your gut microbiome, human cells, and oral microbiome.
Health Intelligence™ — Food + supplement recommendations determined by over 30 health scores and based on an analysis of your gut microbiome & human cells.
Gut Intelligence™ – Food + supplement recommendations determined by over 20 health scores and based on an analysis of your gut microbiome.
Note: I have no personal experience with Viome.
Your Takeaway
An overlooked indicator of and influence on many aspects of your health is the make-up of the microbiota that make up your microbiome.
You actually have more cells in you that aren’t you than those that are you. (You might want to read that last sentence again.) The reason for this is that your microbiome is built with about ten times more bacterial cells — an estimated 100 trillion — than the human cells that make up your body. Given that, it’s very important to understand the nature of your symbiotic relationship with these buggies.
Here’s what to do:
- Get tested — learn how your gut bacteria affects your health.
- Feed the critters that support your health — review the list of foods and supplements suggested above.
- Learn more about your microbiome — here’s a bunch of articles I’ve written on the subject.
Last Updated on August 12, 2022 by Joe Garma