You Absolutely Need To Lower Your Blood Sugar, Part 2 — The 10 Step Solution
Follow the 10 step solution to lower your blood sugar, because it’s highly likely that yours is too high and you will pay a steep price during the second half of life.
IF YOU’VE read Part 1 you may be wondering if you need to lower your blood sugar. I certainly did when I read about the recent challenges to long-held acceptable norms.
Turns out that, yes, 100 mg/dL may be now considered prediabetic, but that there are other blood sugar metrics to consider before swear never to eat a carbohydrate again.
Part 1 focused on the symptoms and risk factors associated with having high blood sugar. I touched on body composition, diet, exercise, neuropathy and age — all of which can indicate the potential for high blood sugar. Then I showed you why medical researchers have reset the acceptable blood sugar level lower than it was.
The bottom line is this:
If you’re overweight, over 45 years of age, inactive and eat processed/fast foods then it’s likely that your blood sugar is too high — especially given the new, lower acceptable levels.
You cannot live a long and vital life with high blood sugar. It tends to mess up various biological systems. The American Heart Association says that high blood sugar can damage your heart (and cardiovascular system), nerves, kidneys, eyes, feet, skin, mouth, as well as osteoporosis and Alzheimer’s. (1)
Given that sustained high blood sugar is so damaging and prevalent — and yet can be managed with a few dietary tweaks — it’s a really good idea to find out your various blood sugar metrics and take action to improve them if necessary.
In this article, you’ll discover:
- What blood sugar numbers are “good” and “not so good”;
- Which tests are most revealing;
- My blood sugar story; and
- The 10 step solution to high blood sugar.
Let’s dive in…
The Numbers and The Tests
The three blood sugar metrics that you need to know are:
- Fasting blood sugar,
- Postprandial, and
- Hb1Ac.
Each one depicts different aspects your blood sugar, and they may not all be of equal relevance.
1. Fasting Blood Sugar
It was in reaction to statements like the one made by Dr. Scott Fogle below that convinced me to test my blood sugar and then say,
“Oh, no!”
(Or something to that effect.)
Dr. Folge said this in response to a question asked by someone concerned that a fasting blood sugar level of 100 mg/dL could lead to prediabetic complications:
“Though mainstream medicine once tolerated blood sugars as high as 140 mg/dL as “normal,” we now recognize the substantial cardiovascular, stroke, and cancer risks posed by sugar levels anywhere above 85 mg/dL. Above that level, your tissues are exposed to glucose at concentrations that cause chemical reactions with your body’s proteins and fats called glycation.
“Glycated proteins and fats trigger inflammation and oxidative stress, major enemies of longevity. Virtually all chronic diseases of aging (and aging itself) are accelerated by high glucose levels.
“As blood sugar rises, your risk of dying also goes up by approximately 40% when fasting glucose consistently falls in the range of 110-124 mg/dL. Risk of dying doubles when fasting glucose reaches the range of 126-138 mg/dL. (2)
There’s a lot of info packed into that quote above, so make sure you at least get the gist of it. I’ll underscore part of it by telling you that the Life Extension Foundation (“LEF”) agrees with Dr. Fogle’s admonition not to let your fasting blood sugar exceed 85 mg/dL.
LEF says you should strive for an optimal range: 70-85 mg/dL. (3)
As you’ll read below in “My Bloody Story”, when I first tested my fasting blood sugar it was 110 mg/dL, last week it was 99 mg/dL and this morning it popped up at 105 mg/dL
This is not where I want it to be, but there may be a silver lining for me — and maybe you — as you’ll soon see.
2. Postprandial
A postprandial glucose test is a blood glucose test that determines the amount of glucose in the blood after a meal, typically done two hours after eating.
Normally, blood glucose levels increase slightly after eating. This increase causes the pancreas to release insulin, which assists the body in removing glucose from the blood and storing it for energy.
A two-hour postprandial blood glucose test measures blood glucose exactly two hours after eating a meal, timed from the start of the meal. By this point blood sugar has usually gone back down in healthy people, but it may still be elevated in people with diabetes. Thus, it serves as a test of whether a person may have diabetes, or of whether a person who has diabetes is successfully controlling their blood sugar. (4)
In response to eating, your postprandial blood glucose reading should increase no more than 40 mg/dL above your fasting value. This means if your fasting glucose is 80, your after-meal glucose should be no higher than 120 mg/dL.
My last postprandial glucose test was done in 2012 and came in at 115 mg/dL, which is good, as you’ll see.
3. Hb1Ac
Hb1Ac (or “A1C”) is shorthand for “Glycated Haemoglobin”. It develops when haemoglobin (a protein within red blood cells that carries oxygen throughout your body) joins with glucose in the blood, becoming ‘glycated’.
The American Diabetes Association explains Hb1AC this way:
“Hemoglobin, a protein that links up with sugars such as glucose, is found inside red blood cells. Its job is to carry oxygen from the lungs to all the cells of the body. Glucose enters your red blood cells and links up (or glycates) with molecules of hemoglobin. The more glucose in your blood, the more hemoglobin gets glycated. By measuring the percentage of A1C in the blood, you get an overview of your average blood glucose control for the past few months. Your doctor should measure your A1C level at least twice a year.” (5)
Whereas the fasting blood sugar test indicates your blood sugar in the moment the test is taken, the A1C test gives you a picture of your average blood glucose (blood sugar) control for the past two to three months, and as such is typically provides a better idea of how well your blood sugar plan is working.
So, is HbA1c A Better Measurement of Blood Glucose Health?
In a word, “yes”.
HbA1c is a more reliable measure of average blood glucose levels than are fasting blood glucose or postprandial tests. This is because blood glucose, being a sugary substance, sticks to (or glycates) hemoglobin, a protein found in red blood cells.
Since red blood cells are relatively long-lived, with a turnover of about 3 months, HbA1c (given in percentages) is a good indicator of average blood glucose levels (if you don’t suffer from anemia or a few other blood abnormalities).
Based on HbA1c, one can then estimate his or her average blood glucose level for the previous three months before the test, using one of the following equations, depending on whether the measurement is in mg/dl or mmol/l:
Average blood glucose (mg/dl) = 28.7 × HbA1c − 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c − 2.59
Your health care provider may report your HbA1c test result as eAG, or “average glucose,” which directly correlates to your HbA1c. The eAG may help you understand your A1C value because eAG is a unit of measure similar to what a blood glucose meter provides. A1C is reported as a percent (7% for example) and eAG uses the same units (mg/dl) as does your glucose meters.
What to shoot for?
The American Diabetes Association suggests an A1C of 7%, which translates to an eAG of 154 mg/dL, but more or less stringent glycemic goals may be appropriate for each individual. (See more about this here.)
Click here for chart showing HbA1c and eAG comparisons.
The relationship between A1C and eAG is described by the formula 28.7 X A1C – 46.7 = eAG.The table below comes from Diabetes Pro, and also provides a conversion calculator here.
| HbA1c | eAG | |
| % | mg/dl | mmol/l |
| 6 | 126 | 7.0 |
| 6.5 | 140 | 7.8 |
| 7 | 154 | 8.6 |
| 7.5 | 169 | 9.4 |
| 8 | 183 | 10.1 |
| 8.5 | 197 | 10.9 |
| 9 | 212 | 11.8 |
| 9.5 | 226 | 12.6 |
| 10 | 240 | 13.4 |
My last Hb1Ac test was done in 2012 and came in at 5.3%, which is equivalent to an aEG of 105 mg/dL.
You can get any of these tests done at competitive prices via the Life Extension Foundation blood panels.
My Bloody Sugar Story
One fine morning three-plus years ago, I borrowed my sister’s blood glucose meter, sat down, pricked my finger, dripped a spot of blood on the strip, inserted the strip in the meter and felt my jaw bounce off the table.
I wrote about this before; namely in an article entitled Control Your Blood Sugar With These 4 Tricks and Supplements. The story bears repeating, because high blood sugar is rampant, is pernicious and doesn’t easily fade away into the night.
This is a picture of the blood glucose result (measured in milligrams per deciliter, “mg/dL”) that rang the warning bell:
According to the Life Extension Foundation (“LEF”):
Prediabetes is diagnosed if the fasting blood glucose level is between 100 and 125 mg/dL.
Diabetes is diagnosed if the fasting blood glucose level rises to 126 mg/dL or above.
Moreover, doctors consider any fasting blood sugar between 70 and 100 mg/dl to be normal, but several studies suggest that people whose fasting blood sugar is over 92 mg/dl are more likely to be diagnosed with diabetes over the next decade. (6)
After I reset my jaw, I turned to my sister who was sitting next to me, and before I could blurt it out, she said,
“With your diet and exercise how is this possible?”
The fast answer is that I don’t know. But what I did know is that I would find out if this particular test was an anomaly, and if it wasn’t I was going to move heaven and earth to lower my fasting blood sugar.
After many subsequent tests with the blood glucose meter, I discovered that although the numbers would fluctuate, on average, my fasting blood sugar was high, but my post-meal tests (“prandial”) were very good.
Some research I’ve done suggests that people on very low carb diets, like mine, may have high fasting blood sugar numbers, which is fine as long as the postprandial and HbA1c numbers are good, which mine are.
Acupuncturists and integrative medicine guru Chris Kresser says that very low-carb diets can produce elevated fasting blood glucose levels: (7)
Because low-carb diets induce insulin resistance. Restricting carbohydrates produces a natural drop in insulin levels, which in turn activates hormone sensitive lipase. Fat tissue is then broken down, and non-esterified fatty acids (a.k.a. “free fatty acids” or NEFA) are released into the bloodstream. These NEFA are taken up by the muscles, which use them as fuel. And since the muscle’s needs for fuel has been met, it decreases sensitivity to insulin. You can read more about this at Hyperlipid.
Chris Kresser agrees with LEF, Dr. Fogle and many other medical types who say that the conventionally accepted blood sugar markers need to be lowered.
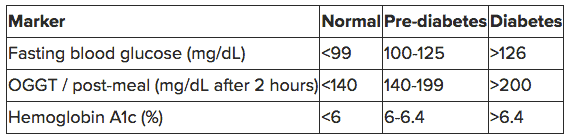
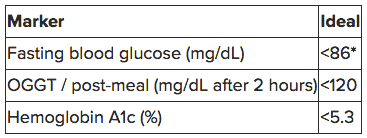
Here’s a table I screen shot from Kresser’s article, Why your normal blood sugar isn’t normal:
This one represents what Kresser and others think should be the blood sugar standard:
At this point, I ask you, Do you think you need to lower your blood sugar?
I did, but my effort proved to be wanting.
A Lackadaisical Effort
Yes, despite my great surprise (and sore jaw) to learn that my fasting blood sugar was at a prediabetic high of 110 mg/dL some three-plus years ago, I did not beat it into submission.
Instead, I was rather lackadaisical.
Perhaps I didn’t really think that 110 was a big deal given that my postpranadial and HbA1c numbers were good, as well as that fine rationale Chris Kresser provided regarding the fasting blood sugar biomarkers for low-carb eaters.
Perhaps all the other moving parts that constitute one’s life intruded.
The bottom line is that I did incorporate some blood-sugar-reducing supplements into my life, such as berberine and amla, but once those supplies were spent I pretty much neglected to monitor my blood sugar, until I began preparing for Part 1 of this two-part blood sugar series.
The morning before I published Part 1 last week, I found my blood glucose meter, jabbed my finger, placed a drop on the strip and held my breath. The number flashed:
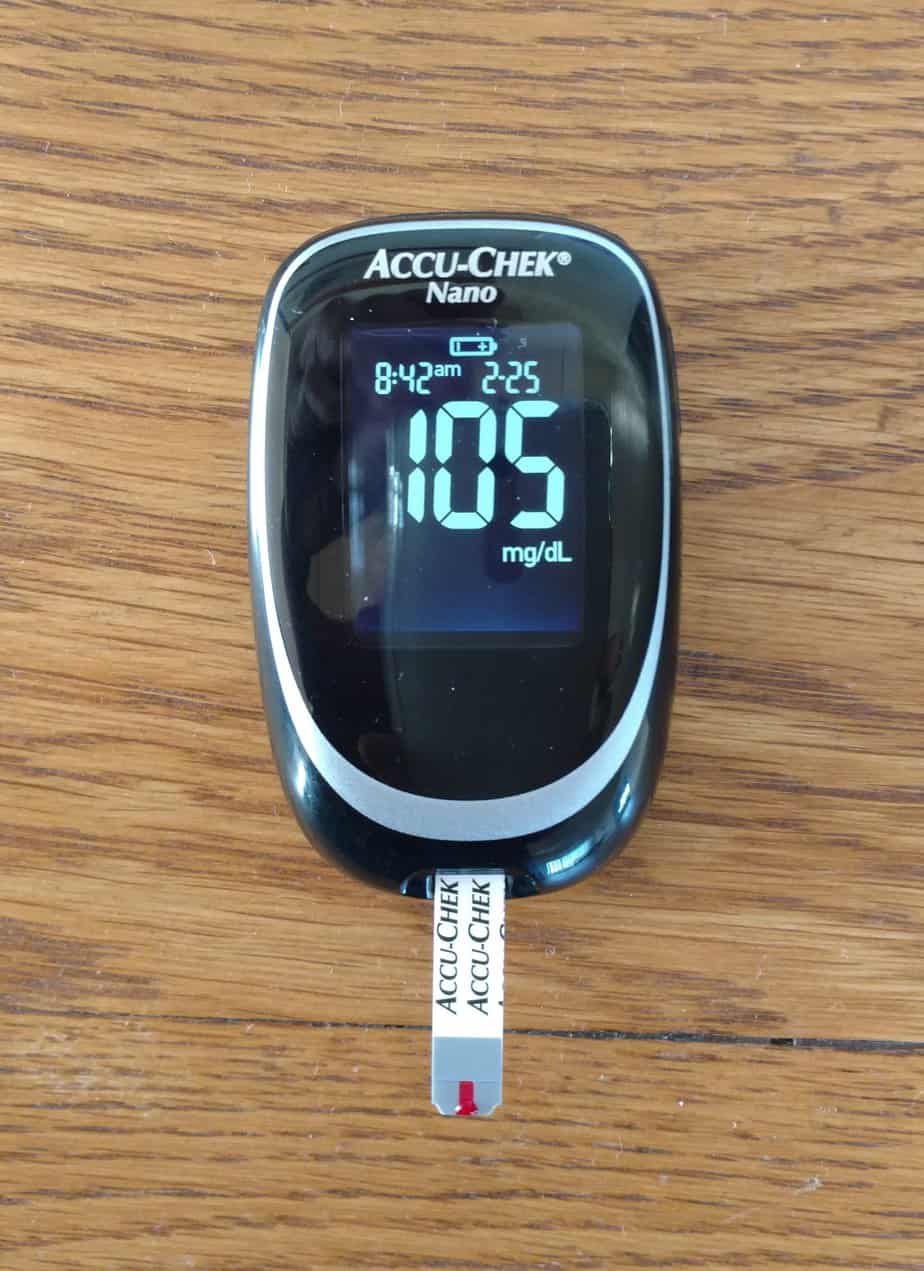
Not great, but going in the right direction — from 110 a few years ago to 99 mg/dL. Yeah, until I checked this morning in preparation for writing this missive. This is a pic of the meter with this morning’s fasting blood sugar number:
Still better than a few years ago, but up from last week.
This really isn’t surprising given that fasting blood glucose can be affected by so many variables that it’s rarely exactly the same in consecutive tests. But whether it’s 110, 105 or 99, my fasting blood sugar results are too high for my comfort, despite the other favorable biomarkers, summarized here:
Summary of Joe’s Blood Sugar Test Results
| Blood sugar test | Joe’s result | Ideal standard | Joe’s score |
| Fasting | 110 mg/dL | 85 mg/dL | + 25 — bad |
| Postprandial | 115 mg/dL | < 120 | On the mark – good |
| Hb1Ac | 5.3% | <5.3% | Real close – good |
My bottom line: I’m somewhat relieved by the favorable postpranadial and Hb1Ac marks, but am invigorated to put the “pedal to the metal” to reduce my fasting blood sugar number.
Next up are the 9 steps I’m going to take to reducing my fasting blood sugar and suggest you consider them as well to lower your blood sugar. (Yeah, there are 10 steps but I’m already doing #1 pretty well.)
Pedal to the Metal — The 10 Steps to Reduce Blood Sugar
1. Reduce simple carbs.
Simple carbohydrates are “simple” because they’re real easy to convert to glucose, the sugar our bodies need to create energy.
You might think it’s a pretty good idea to make creating it’s fuel of preference easy on your body, but it’s just the opposite — you want the carbs you ingest to be slowly converted to glucose so that your pancreas does not have to work hard to produce enough insulin to deal with fast glucose converting carbs.
Simple carbs are typically found in grains, low/no fat processed foods and fast foods. If you’re compelled to eat that bagel, put some almond butter on it so that it’s impact on your blood sugar is lessened. Find ways to make veggies more palatable, such as making smoothies out of them — a handful of spinach, kale, blueberries, almond milk and some high quality protein powder of your choice can do a lot to make consuming veggies more acceptable.
If you exercise, another way to minimize the insulin/blood sugar effects of simple carbs, is to consume them after you exercise. This is when your body needs to restore its glycogen balance and those carbs will be put to good use at that time.
2. Zinc
Zinc, along with the next four supplements (Myo-inositol, Creatine, Berberine and Cinnamon) have been researched by Examine.com and found to have compelling scientific support behind their blood sugar reducing properties. If you get confused about which supplement you should take, do yourself a favor and check out Examine.com’s research which I unabashedly promote here.
In the case of zinc, know this:
- It will only help with high blood sugar if you’re presently deficient in zinc.
- You can get enough zinc by regularly eating meat, fish, beans, nuts, seeds and eggs. I get mine from Brazil nuts.
- Do not pair zinc with minerals like calcium, magnesium, and iron in combined doses of 800 mg or more. You may pair them in lower doses.
- Supplement with 25 – 30 mg per day of “elemental zinc” if you exercise regularly. This “elemental” part is exclusive of, say, zinc gluconate, which improves zinc’s absorption. Thus, to take 30 mg of elemental zinc, take 230 mg of zinc gluconate.
- A daily dose of 10 – 20 mg is sufficient for inactive people.
3. Myo-inositol
Myo-inositol looks similar to glucose, and is a compound that can improve insulin signaling. It’s best to take it with food and to use the powder form, given the suggested amount to consume.
Currently, I’m taking 4 grams of WHC Myo Inositol Powder mixed into my morning shake.
From Examine.com:
- Take myo-inositol with food.
- Try 4 grams if in powder form, or 1,200 mg if it’s a soft gel formulation.
- Pregnant women should not take it, as it could induce uterine contractions.
4. Creatine
Creatine is a source of fuel for muscle cells, which is why many weight lifters supplement with it, including me (though to call me a weight lifter besmirches all who’ve ever hoisted iron). Supplementing with creatine will improve exercise performance and may benefit heart health.
Pertinent to our focus on blood sugar abatement, creatine also improves glucose uptake during muscle contractions, specifically during exercise. Improved glucose uptake gives the muscles more energy to work with and staves off fatigue.
Creatine is a base supplement for glucose uptake and insulin sensitivity because it’s cheap, safe, and does not interact with pharmaceuticals. People with no insulin resistance will still benefit from creatine supplementation.
I use BulkSupplements Creatine. As is suggested for creatine monohydrate (the type you want), I first took a high dose for a week before moving on to a smaller maintenance dose of 5 grams per day, which I tend to take half of before and half after exercise with some water.
From Examine.com:
- The daily dose for creatine is 5 grams a day.
- You will probably want to take it with a meal to lower the risk of an upset stomach.
- If you’re particularly sensitive to creatine’s digestive side-effects, which include nausea and cramping, consider supplementing micronized creatine, which may be gentler on the digestive system.
5. Berberine
Berberine is a compound derived from plants that lowers blood glucose levels by activating a protein called 5 AMP-activated protein kinase (AMPK).
AMPK is responsible for drawing glucose into cells and signaling the body to convert the fuel to energy. This lowers blood sugar levels without interacting with insulin. Berberine supplementation will not cause low blood sugar levels, also known as hypoglycemia, like excess insulin does.
The studies on berberine are pretty compelling.
Consider two studies done on Berberine in 2008. (7)
In one study, newly diagnosed Type-2 diabetics were divided into two groups: berberine and metformin (discussed below) users. Each group consumed 500 milligrams three times a day. These were the results after three months:
- Average fasting blood sugar in the berberine group dropped from 191 to 124 mg/dL.
- Average post-prandial blood sugar dropped from 356 to 199 mg/dL.
- Average hemoglobin A1c dropped from 9.5 percent to 7.5 percent.
- Fasting triglycerides dropped from an average 99 to 78 mg/dL.
- Insulin resistance dropped by 45 percent!
The researchers wrote:
Compared with metformin [discussed below], berberine exhibited an identical effect in the regulation of glucose metabolism, such as HbA1c, FBG [fasting blood glucose], PBG [blood sugar after eating], fasting insulin and postprandial insulin [insulin level after eating]. In the regulation of lipid metabolism, berberine activity is better than metformin. By week 13, triglycerides and total cholesterol in the berberine group had decreased and were significantly lower than in the metformin group (P<0.05).(Source)
These were the results of the berberine group:
- Average hemoglobin A1c decreased from 7.5 to 6.6%.
- Average triglycerides decreased from 221 to 141 mg/dL.
- Average total cholesterol decreased from 205 to 168 mg/dL.
- Average LDL-cholesterol (“bad” cholesterol) decreased from 125 to 97 mg/dL.
There were also positive but modest secondary outcomes (8):
- Body weight decreased by an average of five pounds in the berberine group; whereas the placebo group lost three pounds.
- Systolic blood pressure decreased from an average of 124 to 117 and diastolic blood pressure decreased from an average of 81 to 77 in those treated with berberine, exceeding the fall from 126 to 123 systolic and from 83 to 80 diastolic in those who took the placebo.
I think supplementing with berberine is a no-brainer.
I take 400 mg capsules of Swanson Berberine two or three times per day before meals.
From Examine.com:
- To supplement berberine, take 300 – 500 mg of berberine in three or four divided doses throughout the day, for a total daily dosage of 900 – 2,000 mg. Start at the low end of the range.
- If you have insulin resistance slowly increase the berberine dose to 1,500 mg a day, in three divided doses of 500 mg a day.
- Take berberine with or shortly after a carbohydrate-containing meal. High doses of berberine can cause stomach distress and diarrhea.
- Know that berberine interactions with various enzymes, including CYP3A4, CYP2C9, and CYP2D6. These enzymes metabolize many pharmaceuticals. It is possible that berberine could interact with various oral contraceptives.
6. Cinnamon
Not all cinnamon is the same. The type typically found at your grocers is called Cassia cinnamon, or Chinese cinnamon. Multiple studies indicate that cassia cinnamon can reduce glucose and insulin levels if taken daily. But, according to nutrition expert Dr. Michael Greger, there’s a problem:
Cassia cinnamon “contains a compound called coumarin, which may be toxic to the liver in high-enough doses.” (9)
No problem, let’s use another type of cinnamon called Ceylon cinnamon so you can get the benefits without the potential risks—right? Unfortunately not; although Cassia cinnamon blunts blood sugar, the studies so far done on Celyon show that it’s not as effective.
So, what to do?
Well, what I’m doing it mixing it up. That big bag of cinnamon in the picture above of me at a table filled with blood sugar reducing supplements is Ceylon cinnamon (Frontier brand), and I mix it along with Cassia cinnamon.
Another option is cinnamon tea. Although brewing tea makes it difficult to supplement precise dosages, cinnamon tea contains less coumarin than cinnamon supplements. The tea reduces the risk of coumarin poisoning because the toxin is left behind in the dregs.
From Examine.com:
- To supplement cinnamon, take 5 – 6 g of Ceylon cinnamon, or Cassia cinnamon.
- Cinnamon should be taken throughout the day, with meals containing carbohydrates.
7. Amla
I wrote about Amla in Eight Steps To Get More Sex and A Longer Life by Supercharging Your Blood. I’ll repeat some of it.
Also called “Indian Gooseberry”, Amla just might be the biggest bang for your blood sugar lowering buck. In fact, the aforementioned Dr. Michael Greger of NutritionFacts.org says: (10)
Am I recommending people treat their diabetes with gooseberry powder? No, I recommend curing your diabetes… Why treat anything when you get at the root cause and reverse it in the first place.
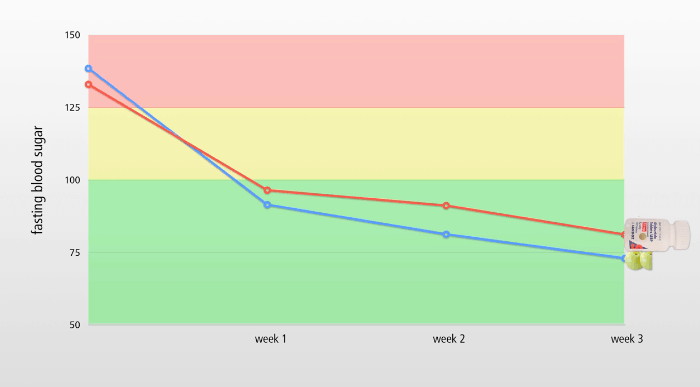
Take a look at the graph below. It depicts the results of a study measuring the effect of Amla fruit on blood glucose and lipid (fat) profiles of Type-2 diabetic and non-diabetic participants. (11, 12)
The blue line depicts the fasting blood sugar levels of the participants on diabetic medication, glyburide (sold as Diabeta or Micronase), and the red line shows those taking Amla.
At the beginning of the study, participants in each group (glyburide and Amla) have very high blood sugar levels, above 125 mg/dL, which by definition is a diabetic level. (100 to 125 is pre-diabetic; normal is below 100, but ideally should be below 90 — 85 says LEF.) (13)
Effect of Diabetic Medication and Amla on Fasting Blood Sugar
Note that both the medication and Amla were very effective at quickly reducing fasting blood sugar to acceptable levels (under 100 mg/dL) within the first week, and then dropped it further over the subsequent two weeks, with Amla outperforming the drug.
You can use diabetes medication, most of which are now generic, and spend about $18 per month and face side effects such as weight gain, vomiting, liver disease or bone marrow poisoning. Or you can use gooseberries, which cost less than $5 for a month’s supply (powdered form) and has the side effect of sourness. (14)
Dr. Greger says that even taking one-quarter of a teaspoon a day can normalize blood sugar, but I’m a glutton — I take a tablespoon in my morning shake. UPDATE: Am splitting the dose, one teaspoon in the morning with my morning shake and one teaspoon after dinner. Currently, I’m using Feel Good Organic Amla Powder.
8. Apple cider vinegar
As NutritionFacts.org reports, a double blind, placebo-controlled, randomized study found that body weight and belly fat were significantly reduced by adding just a single tablespoon of vinegar to your daily diet.
All by itself, that’s enough for me, but there’s more!
On two tablespoons per day, those in the study experienced normalized triglycerides and a dip in blood pressure, although this could be due to the drop in weight rather than something uniquely attributable to the vinegar.
But we’re here to learn about how to reduce blood sugar, and that’s why my weary fingers must continue pecking away, because if you chug down four teaspoons of apple cider vinegar diluted in water, you can blunt a post-meal sugar spike by half. (15)
I say: Develop a taste for apple cider vinegar.
I take a tablespoon (three teaspoons) of apple cider vinegar in a large glass of pure water before I consume any high-carb meal, and often before bed as well. The brand I use is Trader Joe’s unfiltered apple cider vinegar.
9. Fiber
WebMD says that women need 25 grams of fiber a day, and men need 38, but that most of us only get 15 grams a day.
Can anyone spell “C-O-N-S-T-I-P-A-T-I-O-N?
Being “regular” is a mighty fine thing, but to continue with our prediabetes theme here, know this about fiber in your diet
Prevention.com tells us that it takes 10 grams of fiber to reduce by 25% the blood sugar surge from consuming a serving of starch. No single, typical serving of fruits or vegetables comes close to providing the 10 grams needed to lower your blood sugar by 25%. So, you either need to eat more like a gorilla, or sprinkle some fiber in your water or on food.
I do both. Top sources of fiber I consume are: beans (all kinds, soaked and sprouted), peas, chickpeas, black-eyed peas, artichokes, raspberries, blackberries, and prunes.
And then there’s Tri-Cleanse. This is a blend of fibers and herbs with the “legendary Triphala compound of India”. I make sure I consume about a tablespoon of Tri-Cleanse mixed into a large glass of water and lemon on any day that I’m not eating enough fibrous foods.
10. Metformin
There’s much to say about Metformin.
It’s been used successfully for many years to control diabetes, but is now being investigated as an anti-aging drug.
I wrote about this in Do These 2 Anti-aging Pills Really Work?, which I wholeheartedly recommend you read for the longevity angle.
As concerns high blood sugar, know this:
- Scientists are reviewing whether Metformin use can possibly improve the gene expression profile in older adults with damaged glucose tolerance to that of younger individuals.
- What is known is that Metformin increases the number of oxygen molecules released into a cell, and this appears to boost robustness and longevity. It works by suppressing glucose production in the liver and increasing insulin sensitivity, therefore benefiting patients with type 2 diabetes. (15)
I’ve been stroking my chin as I’ve read the many studies about Metformin. I’m thinking that at some point I might try it in a low dose, not only for blood sugar management, but for the aging angle as well.
Your Takeaway
Remember these three things that will help lower your blood sugar, and then, step by step, incorporate them into your life:
- If you really do not want high blood sugar to become your chronic health problem to deal with as you age, you probably need to reduce your blood sugar. Get tested and if it’s higher than the ideal numbers presented above, get invigorated and try some of the supplements I covered.
- Favor complex carbs over simple carbs. This means, eat carbohydrates that do not spike blood sugar. Complex carbs come from veggies, legumes and whole grains. If you’re not a fan of vegetables, get into a smoothie habit, whereby you add the veggies along with some protein powder and whatever other tasty — but not garbage — morsels you like.
- Pick a blood sugar blunting supplement and use it. Then add another.
You can expect another article on this topic from me some day, because I’m gonna want to crow about my new, low fasting blood sugar. Stay tuned for that!
Last Updated on March 1, 2022 by Joe Garma