Lesson 6: Reduce Baseline Inflammation With A Nutritious Anti-inflammatory Diet
Lesson 6 Protocol 2
Adopt an anti-inflammatory diet rich in omega 3 fatty acids, vegetables, whole fruits, lentils and beans.
The most important three things you can do to reduce chronic baseline inflammation are all related to diet.
Put some effort in these:
- Glycemic control
- Learn the glycemic load of the foods you eat regularly.
- Eat less or avoid those with a high glycemic load.
- Microbiome balance
- You can’t be healthy if the beneficial bacteria in your gut and elsewhere are not dominant.
- Feed the beneficial bacteria by consuming short chain fatty acids (SCFAs), which are high in dietary fiber.
- Foods high in dietary fiber include beans, lentils, avocados, chia seeds, acorn squash, green peas, collard greens, broccoli, oranges, and sweet potato.
- Dietary nutrition
- Avoid eating processed and sugary foods, drinks and (sigh) alcohol.
- Eat foods from the anti-inflammatory food pyramid.
Reduce Baseline Inflammation With A Nutritious, Anti-inflammatory Diet
Improvements in diet are strongly associated with reductions in inflammation. If you want to enhance your immunity to COVID-19, what you eat needs to be a primary focus.
The three focal points regarding a nutritious diet are:
- Glycemic control
- Microbiome balance
- Dietary nutrition
Glycemic Control
“Glycemic” literally means "causing glucose in the blood." And Glycemic control is about keeping your blood sugar from spiking. Insulin resistance, obesity, and impaired glucose tolerance are all associated with inflammation. [1,2,3]
Blood glucose levels are closely related to the amount and type of carbohydrates you consume.
Carbs that are highly processed are referred to as “refined carbs” and they’re often high in sugar. Refined carbs are high-glycemic foods, because for most people they cause a blood glucose spike. When blood glucose rises, the pancreas has to produce more insulin to bring the sugar into cells for energy, or to store it as fat if that energy isn’t needed right away.
Not everyone’s blood sugar reacts the same to the same foods, but for most of us, Captain Crunch cereal spikes our blood sugar and a sweet potato, although “sweet”, doesn’t.
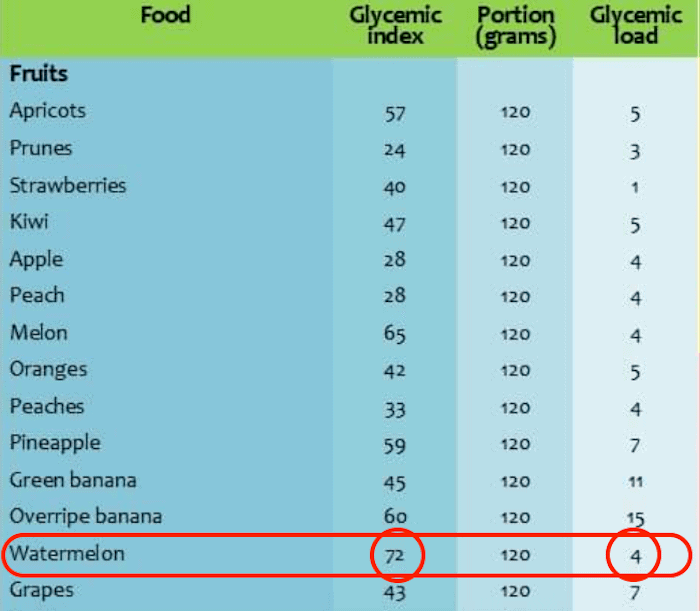
There’s an index of foods that lists their relative impact on blood sugar level two hours after consuming a particular food. It’s called the Glycemic Index. And there’s one that lists the Glycemic Load of various foods.
The difference between the two is worthy of your attention.
The glycemic index assigns a numeric score to a food based on how drastically it makes your blood sugar rise. Foods are ranked on a scale of 0 to 100, with pure glucose (or sugar) given a value of 100.
The lower a food's glycemic index, the slower blood sugar rises after eating that food. In general, the more processed a food is, the higher its GI, and the more fiber or fat in a food, the lower its glycemic index.
But the glycemic index tells just part of the story. What it doesn't tell you is how high your blood sugar could go when you actually eat the food.
To understand a food's complete effect on blood sugar, you need to know both how quickly it makes glucose enter the bloodstream, and how much glucose per serving it can deliver.
A separate measure called the “glycemic load” does both, and it gives you a more accurate picture of a food's real-life impact on your blood sugar. Focus on glycemic load, not the glycemic index.
Watermelon has a high glycemic index -- 80 out of a maximum level of 100 -- but a serving of watermelon has so few carbohydrates that its glycemic load is below 10. This is not typical, as more often foods that have a high glycemic index also have a high glycemic load.
If you’re overweight or have high blood sugar, it could be that you eat too much of high glycemic foods too often. I suggest you check the glycemic load of the packaged foods you eat.
There’s a link to a glycemic index and load chart in the References tab.
Now let’s turn to the second dietary focal point, the feeding of your microbiome.
Microbiome Balance
What’s a “Microbiome” and what does it do?
- The microbiome is the community of microorganisms (microbiota) living together in and on you.
- The microbiota are integral to the regulation of our metabolism, influencing how our muscles, liver and fatty tissue use and store energy, and much more.
- Dysregulation of a balanced microbiome in your gastrointestinal tract can cause systemic inflammation.
You might get squeamish to hear me say this, but your lungs and GI tract host a microbiome populated by microbiota, or to put it the common parlance… bacteria.
We’re talking trillions of these critters. They have a complex relationship with the lungs and GI tract, and a bidirectional relationship with your immune system.
Dysregulation of the balance of GI microbiome bacteria has been shown to be a source of systemic inflammation. [4,5.6,7]
“Dysregulation” refers to the impairment of a normal physiological response to something. In this context, dysregulation refers to a disruption of the normal, healthy symbiotic relationship between the microbiota that live in the lungs and GI tract, and those that live in both.
To keep dysregulation of the microbiome from increasing inflammation, eat dietary fiber. Dietary fiber increases short chain fatty acids (SCFAs), specifically one called propionate.
Propionate is among the most common short-chain fatty acids produced by human gut microbiota in response to indigestible carbohydrates, which are also referred to as fiber in the diet. These dietary fibers consist of a group of complex carbohydrates found mostly in vegetables, fruits and legumes. Propionate has been shown to enhance the production of macrophages and dendritic cells in the lungs, which is what we want to occur to improve our immunity.
Macrophages are white blood cells that locate microscopic foreign bodies and 'eat' them by using the process of phagocytosis to engulf and digest them. Dendritic cells capture the antigens from invading bodies.
Antigens are molecules capable of inducing an immune response, which is to produce an antibody in the host organism. So, the dendritic cells process and then present the antigens on their cell surface, and that promotes B cell activation. B cells are lymphocytes that are responsible for producing and releasing antibodies to specific antigens.
This is a big part of how our immune system works, and speaks to the value of dietary fiber in our diets, which help produce those short-chain fatty acids, like propionate.
The bottom line with lung and GI microbiota is that you want to feed them plenty of dietary fiber in the form of complex carbs so that they can function properly.
This is especially important in situations requiring the use of ventilators. For instance, it’s been shown that a depletion of the lung microbiota by broad-spectrum antibiotics prior to ventilation was shown to render mice more susceptible to developing ventilator-induced lung injury. This is because antibiotics kill beneficial microbes in our bodies.
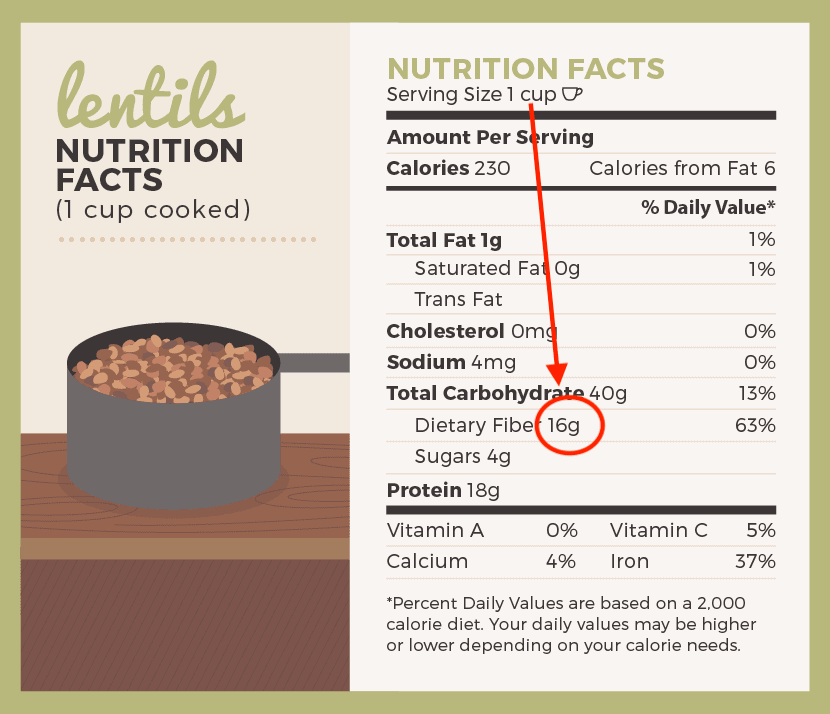
I realize you’re not a mouse, but our genomes are much alike, so eat your dietary fiber. Shoot for 25 to 30 grams per day. Foods that come in containers show the fiber number on the labels.
Here’s an example that shows how much fiber is in lentils:
Make a habit of checking the fiber content of the food you buy. In addition to lentils, other high fiber foods include beans, avocados, chia seeds, acorn squash, green peas, collard greens, broccoli, orangea and sweet potato.
Now, let’s examine the nutritional factors that will enhance your immune response by reducing baseline inflammation.
Dietary nutrition
It’s undeniable that improvements in dietary nutrition are strongly associated with reductions in inflammation.
A 2006 study published in the Journal of American Cardiology said that:
“Dietary patterns high in refined starches, sugar, and saturated and trans-fatty acids, poor in natural antioxidants and fiber from fruits, vegetables, and whole grains, and poor in omega-3 fatty acids may cause an activation of the innate immune system, most likely by an excessive production of proinflammatory cytokines associated with a reduced production of anti-inflammatory cytokines.” [8]
This is the essence of what’s going wrong with the immune systems of many people who get sick from COVID-19 -- their immune response to the infection and resulting disease is too proinflammatory.
The relationship between dietary quality and the immune system is especially important to us as we get older. As you know, the elderly are among the most vulnerable to COVID-19 illness.
Immune response declines with age, and many older adults have chronic low-level inflammation and underlying health conditions, like heart disease, high blood pressure and diabetes -- all of this challenges the body’s defenses.
Your diet needs to be nutrient-dense. Numerous studies have clearly shown that a healthful, whole foods plant-based diet enhances your immune function at any age. There are thousands of substances in fruits, vegetables, whole grains, legumes, and soy products that are protective against infections.
Such foods are the basis of the anti-inflammatory diet I’ll share with you in a minute, but first let’s take a look at foods that are inflammatory and those that reduce systemic inflammation.
Avoid these inflammatory foods:
- Fried foods
- Sodas
- Refined carbs
- Processed meats
- Margarine and shortening
- Alcohol
Avoid Fried foods
Restaurants and packaged foods companies tend to use hydrogenated oils, margarine and shortening to get a perfectly crisp French fry, or piece of fried chicken.
These fats contain trans fatty acids, and can cause inflammation of the endothelium, which is the thin inner lining of your heart and blood vessels. [9]
Your entire circulatory system is lined with these cells. They manage the exchange of nutrients and toxins between nearby tissue and the bloodstream.
Inflammation of the endothelium is associated with a long list of diseases, including heart disease, diabetes and insulin resistance. [10]
The science clearly backs this up. In a study of more than 100,000 women, those who ate a daily serving of fried chicken were 12% more likely to die from heart-related health issues. And those who ate fried fish or shellfish daily were 13% more likely to die from the same causes. [11]
Instead of eating fried foods, do this instead:
- Avoid fried foods. You can still achieve delicious results with other cooking methods, like baking and using an Air Fryer.
- If you’re going to eat fried foods, opt for quality, high-heat cooking oils like ghee or avocado oil. These fats have a better fatty acid profile than vegetable oil or canola oil.
Avoid Sodas
Soda either contains sugar or some sugar substitute, most of which are nasty and inflammatory.
Your body recognizes artificial sweeteners as a toxin and stores it in the fat tissue where it generates an inflammatory response. Your body attempts to dilute the chemical with water, causing added water weight in the body.
Even if you avoid artificial sweeteners, the amount of sugar in regular soda is enough to cause your body to feel puffy.
A single 12 ounce can of cola contains almost ten teaspoons of sugar. As your body processes glucose, which is a type of sugar, it will store at least three grams of water for every gram of glucose, leading to excess water-weight.
And just like trans fats, fructose (another type of sugar) can cause inflammation of the endothelium.
Instead of soda, drink Carbonated Water:
- If it’s the carbonation you crave, try sparkling water flavored with natural fruit essences. Check out the La Croix, Waterloo and Spindrift brands.
- Try eight ounces of unflavored sparkling water with one or two tablespoons of unfiltered, organic apple cider vinegar. If your sweet tooth complains, add a small amount of a healthy sugar substitute, such as Stevia, Xylitol, or my favorite, Erythritol.
Avoid refined carbohydrates
White bread, pizza dough, pasta and pastries are often made with white flour. Everything that may have had a bit of nutrition in the wheat is stripped out of white flour, such as the fiber and bran.
This process robs the wheat of the few nutrients it has, and leaves behind the carbohydrates.
Your body quickly breaks down refined carbohydrates into sugar, exposing you to the same inflammatory risks caused by sugar as mentioned above.
For most of us, eating a high-carb meal causes a glycemic spike. In response, more insulin is produced and this can lead to a state of oxidative stress that is inflammatory. [12]
Your body’s metabolic processes are designed to break down whole, fibrous foods. When your gut microbes go through the time-intensive process of separating cellulose from the simple carbohydrate, they consume some of the glucose. This keeps your body from producing the insulin spike it gets from consuming refined carbohydrates devoid of fiber.
A diet of refined carbohydrates cheats your gut microbiota of the benefits they get from breaking down complex carbohydrates, and you get more inflammation. [13]
Instead of eating refined carbs, do this instead:
- Avoid foods made with refined flour, such as white bread, pastries, packaged snacks and pasta.
- If you eat grains, opt for whole grains like quinoa, buckwheat and oats.
Avoid processed meats
Processed meats are preserved with nitrates and nitrites. These are simple organic compounds made of nitrogen paired with two or three oxygen atoms.
In the process of digestion, nitrates typically lose an oxygen molecule and thereby become nitrites. This adds to your body’s oxidative stress.
Nitrites are the same molecules found organically in vegetables like spinach, kale and cabbage. In these foods, nitrites are healthy. However, they transform into dangerous nitrosamines when they are cooked in the presence of protein. These nitrosamines generate oxidative stress and inflammation. [14]
Even meats labeled as “uncured” or “no nitrites added” contain nitrites. These foods get their nitrites from celery, beets or another natural source that’s used in the curing process. [15]
Whether sourced from nature or from man-made sodium nitrite, the molecule is the same — and when cooked with meat, either one is just as inflammatory as the other.
By the way, smoked meats also include PAHs (polycyclic aromatic hydrocarbons) and HCAs (heterocyclic amines), which both promote cancer.
Rather than eating processed meats, do this instead:
- Cut back on processed meats, like bacon, and when you do eat them eat pasture-raised varieties from reliable sources.
- If you have to eat bacon, choose pasture-raised bacon, and minimize oxidation by cooking it at lower temperatures — i.e. don’t burn it.
Avoid Margarine and shortening
Once upon a time, butter was made out to be the villain and margarine and shortening were presented as healthier choices. They’re not! They're made of trans fats, which are pro-inflammatory.
Rather than eating margarine or shortening, do this instead:
- Cook with quality fats like avocado oil, olive oil, or grass-fed butter.
- Drizzle avocado oil or cold pressed virgin olive oil on your toast, or grass-fed butter.
Avoid Alcohol
Ever felt a little puffy after tossing back a few servings of alcohol? That’s what acute inflammation feels like.
This pandemic we’re experiencing has caused a serious spike in alcohol sales. If you’re among those who are drinking more than one or two servings of alcohol per day, I suggest you push back against this tendency, because drinking alcohol will inflame your body, the opposite of what you want during this pandemic.
Alcohol leads to inflammation in your body two ways:
- First, alcohol causes DNA damage to your body’s cells, which engages an inflammatory response as the cellular clean-up crew arrives.
- Second, the damage to the liver causes inflammation, abdominal swelling and bloating, as well as a host of other negative health and cognitive effects.
If you drink regularly, your body generates endotoxins that trigger inflammation, and it remains in this heightened state of inflammation, which not only might predispose you to an excessive inflammatory response to the coronavirus, should you get infected, but also can contribute to chronic disease.
The bottom line is that we must be careful with how much alcohol we consume.
Alcohol inflames the body, which is contrary to our goal of improving the effectiveness of our immune system, in part, by reducing baseline, or chronic inflammation.
The Anti-inflammatory Diet
Now that you know the inflammatory foods you don’t want to eat, let’s turn to foods that fight inflammation.
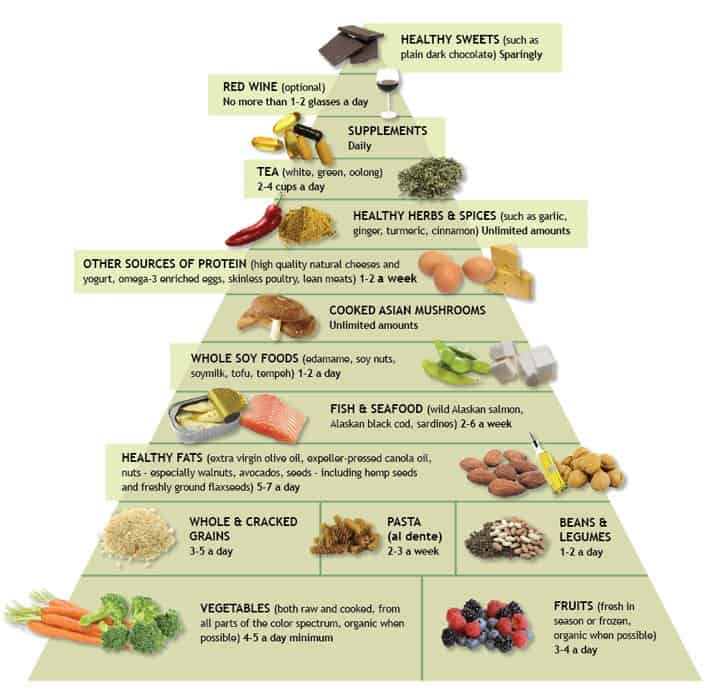
There are many wholesome foods that support a healthy inflammation response in your body, and Dr. Andrew Weil made an Anti-inflammatory Food Pyramid to guide you.
Dr. Weil is the Founder and Director of the Program in Integrative Medicine at the University of Arizona in Tucson. He’s devoted decades of his life to studying how to work with the body’s natural systems for healing.
Here’s his pyramid:
(Check out Dr. Weil’s interactive Anti-inflammatory Diet Pyramid.
Dr. Weil recommends that the average diet should consists of the following macronutrient proportions:
- 40 to 50% carbohydrates,
- 30% from fat (particularly omega-3 fatty acids)
- 20 to 30% from protein (particularly low mercury fish and grass fed meat).
There’s nothing set in stone about these proportions. Some individuals will do better with different ratios of macronutrients.
For instance, those who regularly lift weights or do calisthenics may require more protein, which is needed to repair the microtears in muscle fiber that resistance exercise can do. It’s this repair process that makes the muscles larger and stronger.
Those who regularly run, bike or swim for an hour or longer -- all examples of aerobic exercise -- may require more carbohydrates.
The fundamentals of the anti-inflammatory diet include boosting fruit and vegetable intake, seeking out fresh food, avoiding refined sugars, eating healthy fats from cold pressed extra-virgin olive oil and avocado oil, eating cold-water, oily fish such as wild-caught salmon, choosing foods high in antioxidants and omega-3 fatty acids and decreasing processed foods.
This diet provides abundant vitamins, minerals and fiber; facilitates stable blood-sugar levels; and helps to control the inappropriate inflammation that underlies many of the developed world’s chronic diseases including Alzheimer’s and Parkinson’s diseases, heart conditions and many cancers --- and it supports our goal of reducing baseline inflammation.
I encourage you to spend some time with the pyramid on the interactive site. Click on each food category and see what’s recommended. Then let your grocery shopping and the meals you make reflect this guidance so that you can reduce your baseline inflammation and be more resilient to Covid.
To get you started, check out Consumer’s Reports Anti-Inflammatory Diet: 9 Recipes to Get You Started. Youtube also has thousands of videos that show you how to prepare anti-inflammatory meals.
If you’d like to dig deeper into the assertions I’ve made about the impact of nutrition on chronic inflammation, check out References 16 -- 22 in the Reference Tab.
Your Takeaway
The three areas you need to focus on concern:
- Glycemic control
- Learn the glycemic load of the foods you eat regularly.
- Eat less or avoid those with a high glycemic load.
- Microbiome balance
- You can’t be healthy if the beneficial bacteria in your gut and elsewhere are not dominant.
- Feed the beneficial bacteria by consuming short chain fatty acids (SCFAs), which are high in dietary fiber..
- Foods high in dietary fiber include beans, lentils, avocados, chia seeds, acorn squash, green peas, collard greens, broccoli, oranges, and sweet potato.
- Dietary nutrition
- Avoid eating processed and sugary foods, drinks and (sigh) alcohol.
- Eat foods from the anti-inflammatory food pyramid.

Leave a comment
Comment as a guest: